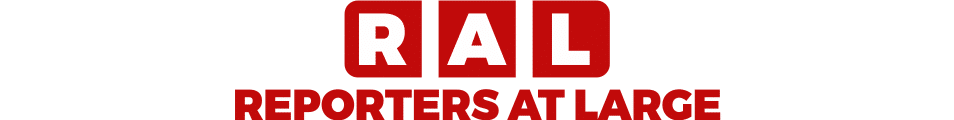
Diabetes is a chronic condition characterised by elevated blood sugar levels due to the body’s inability to produce or effectively use insulin. There are three primary types of diabetes: Type 1, Type 2, and gestational diabetes, each exhibiting different causes, symptoms, and management strategies.
Type 1 diabetes, often diagnosed in children and young adults, occurs when the immune system mistakenly attacks insulin-producing beta cells in the pancreas. This results in little to no insulin production, necessitating lifelong insulin therapy. Common symptoms of Type 1 diabetes include excessive thirst, frequent urination, extreme fatigue, and blurred vision. Early diagnosis is crucial, as untreated Type 1 diabetes can lead to severe complications, including ketoacidosis.
Conversely, Type 2 diabetes is more prevalent and generally develops in adults, though it has been increasingly diagnosed in younger populations due to lifestyle factors. In Type 2 diabetes, the body becomes resistant to insulin, or the pancreas fails to produce sufficient insulin. Symptoms may mirror those of Type 1, but can also include slow-healing sores, frequent infections, and areas of darkened skin (acanthosis nigricans). Recognising these symptoms promptly is vital for implementing effective management strategies.
Gestational diabetes occurs during pregnancy and typically resolves after childbirth, although it may predispose individuals to Type 2 diabetes later in life. Hormonal changes during pregnancy can impair insulin’s effectiveness, resulting in elevated glucose levels. Symptoms may be subtle or absent, making routine screening essential for early detection.
Risk factors for diabetes include family history, sedentary lifestyle, obesity, and unhealthy dietary habits. Unmanaged diabetes can result in serious complications, such as heart disease, nerve damage, kidney failure, and vision loss. Understanding the types of diabetes and their symptoms is crucial for early detection and intervention, which can help mitigate long-term health risks.
The Role of Diet in Diabetes Management
Diet is a fundamental aspect of diabetes management, as it plays a crucial role in regulating blood glucose levels and supporting overall health. Adopting a diet rich in whole foods is highly recommended. Whole foods are minimally processed and retain their natural nutrients, which can help stabilise blood sugar levels. Emphasising fruits, vegetables, whole grains, and lean proteins is essential in crafting a diabetic-friendly diet. Moreover, opting for low-glycaemic index (GI) foods can further assist in controlling blood sugar spikes. These foods are digested and absorbed slowly, preventing sudden increases in glucose.
Incorporating fibre into the diet is another effective strategy. Dietary fibre in legumes, vegetables, and whole grains helps improve digestion and moderate blood sugar levels. High-fibre foods can promote a sense of fullness, thereby reducing overall calorie intake, which is particularly beneficial for those with weight management concerns often associated with diabetes. Healthy fats are also essential; they can be sourced from avocados, nuts, and olive oil. These fats support heart health, which is vital as individuals with diabetes are at an increased risk for cardiovascular disease.
Protein also plays a significant role in blood sugar regulation. Including protein-rich foods such as chicken, fish, and plant-based proteins can contribute to a balanced meal that provides sustained energy without causing rapid spikes in glucose levels. It is equally important to avoid processed sugars and refined carbohydrates, as these can lead to significant fluctuations in blood sugar levels. Establishing healthy eating habits, planning meals, and being mindful of portion sizes can help maintain stable glucose levels. Overall, a well-structured dietary approach can be a powerful tool in managing diabetes.
Herbal Remedies and Supplements
Managing diabetes effectively often demands a multifaceted approach, including attention to diet, lifestyle, and, importantly, herbal remedies and dietary supplements. Several natural options have gained prominence in diabetes management due to their potential to lower blood sugar levels. Cinnamon, bitter melon, berberine, and fenugreek are particularly noted for their efficacy.
Cinnamon, a common spice, has been shown in various studies to enhance insulin sensitivity and lower fasting blood sugar levels. Research indicates that cinnamon constituents, such as hydroxychalcone, may mimic the action of insulin, facilitating glucose uptake by cells. This makes cinnamon a flavourful addition to meals and a promising candidate in the natural management of diabetes.
Another noteworthy herbal remedy is bitter melon, often celebrated in traditional medicine for its anti-diabetic properties. Studies have shown that bitter melon contains compounds that function similarly to insulin, effectively lowering blood sugar levels. Additionally, this fruit is rich in vitamins and minerals, further contributing to overall health.
Berberine is a bioactive compound found in several plants, such as goldenseal and barberry, that has garnered attention for its ability to regulate glucose and lipid metabolism. Research has demonstrated that berberine can significantly reduce blood sugar levels and improve insulin sensitivity, making it a potential supplement for those managing diabetes.
Lastly, fenugreek seeds are another herbal supplement that has shown promise in controlling blood sugar levels. These seeds are rich in soluble fibre, which may help to slow the absorption of carbohydrates and improve glucose tolerance, thus aiding individuals with diabetes in maintaining better control over their condition.
While these natural treatments offer promising benefits, it is essential to approach them with caution. Potential side effects or interactions with prescribed diabetes medications are possible, and therefore, consulting a healthcare provider before incorporating any herbal remedies or supplements into a treatment plan is strongly advised.
Lifestyle Changes to Enhance Diabetes Management
Managing diabetes effectively extends beyond dietary considerations; lifestyle changes enhance overall health and maintain stable blood sugar levels. One of the foremost strategies is engaging in regular physical activity. Exercise not only aids in weight management but also improves insulin sensitivity, allowing the body to utilise glucose more efficiently. At least 150 minutes of moderate aerobic exercise weekly, such as brisk walking or cycling, can significantly enhance diabetes control. Additionally, strength training should be included at least twice a week to build further muscle mass, which is beneficial for metabolic health.
Another crucial aspect of diabetes management is stress reduction. Chronic stress can lead to elevated blood sugar levels due to the release of stress hormones, such as cortisol, which can interfere with insulin function. Mindfulness techniques, such as meditation, yoga, or deep breathing exercises, can help alleviate stress and improve emotional well-being. Setting aside time each day for these practices can cultivate peace and help regulate blood glucose levels more effectively.
Moreover, ensuring adequate and quality sleep is indispensable for individuals managing diabetes. Lack of sleep disrupts hormonal balance and can lead to insulin resistance. Striving for 7-9 hours of sleep per night is essential; establishing a consistent sleep routine and creating a calming bedtime environment can foster better sleep hygiene. By prioritising these lifestyle changes—regular exercise, stress management, and sufficient sleep—individuals can take a proactive approach to diabetes management, improving insulin sensitivity and overall health.